Q Wave – What Is It? And Its Importance In Pathology
Q wave abnormalities are often associated with myocardial infarction.
Author:Suleman ShahReviewer:Han JuJun 25, 202245 Shares890 Views

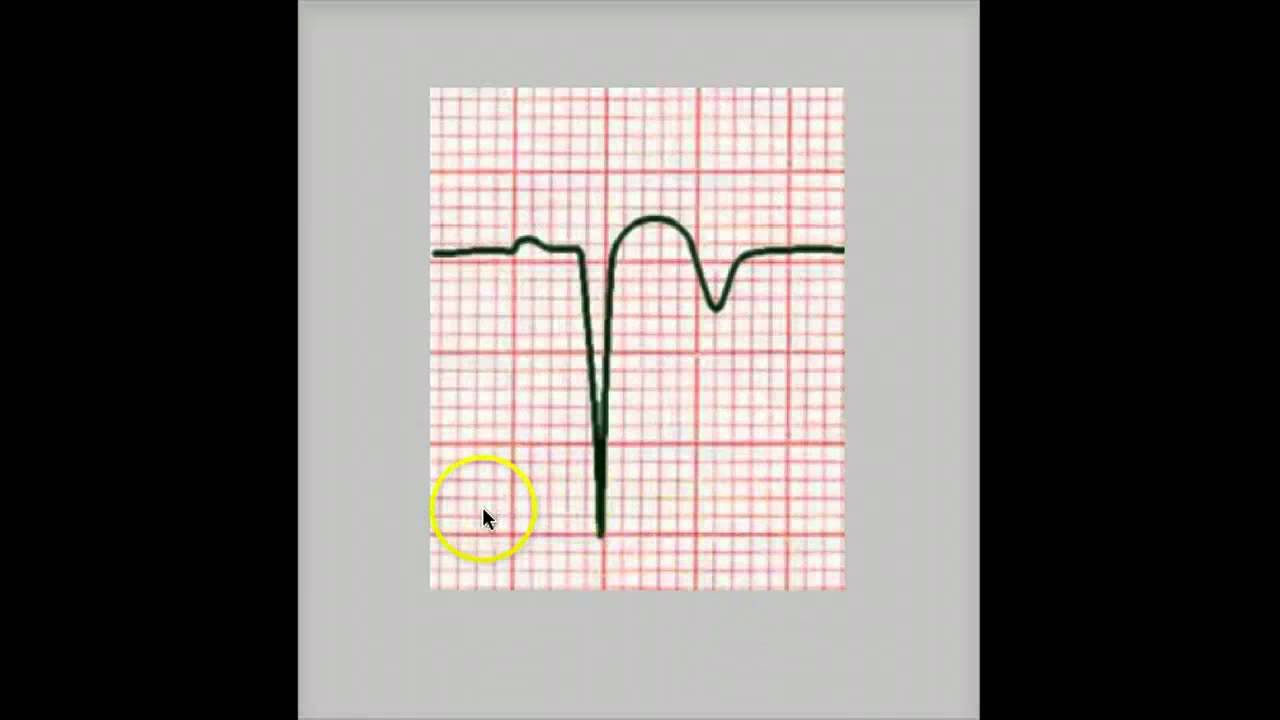
The QRS complex begins with the Q wave, the first downward deflection following the P wave. There is no Q wave when the initial deflection of the QRS complex is vertical. In many, but not all, ECG leads, a typical person will have a modest Q wave.
Q wave abnormalities are often associated with myocardial infarction. The names "Q wave myocardial infarction" and "non-Q wave myocardial infarction" was formerly used to describe various kinds of MIs that resulted in either Q wave development or the lack of Q wave development.
Q wave in ECG
Pathological Q Waves
Pathologic Q wavesindicate a prior myocardial infarction. A lack of electrical activity causes them. A myocardial infarction may be seen as an electrical 'hole,' since scar tissue is electrically dead, resulting in pathologic Q waves. Pathologic Q waves are not an early indicator of myocardial infarction; they often develop over many hours to days. Once pathogenic Q waves have formed, they seldom disappear. If the myocardial infarction is reperfused early (for example, as a consequence of percutaneous coronary intervention), shocked myocardial tissue may recover and pathologic Q waves dissipate. In all other cases, they normally last eternally.
The exact definition of pathologic Q waves has been questioned. Any Q-wave in leads V2-V3 0.02 s or QS complex in leads V2 and V3 Q-wave 0.03 s and > 0.1 mV deep or QS complex in any two leads in a contiguous lead grouping (I, aVL,V6; V4-V6; II, III, and aVF).
In the absence of a conduction defect, R-wave 0.04 s in V1-V2 and R/S 1 with a concordant positive T-wave.
PATHOLOGIC Q WAVE
Normal Q Wave
More than 75% of ordinary people have small Q waves in their left precordial leads. They are most common in lead V6, less often in leads V5 and V4, and seldom in V3. Q waves in these leads are more common in younger participants than in older people. When the transitional zone lies on the right side of the precordium, Q waves are more likely to be present. The Q waves last no more than 0.03 seconds. The amplitude is typically less than 0.2 mV, although it may reach 0.3 mV or even 0.4 mV. Young adults get deeper Q waves more often. 22 Teenagers may experience amplitudes of 0.4 mV or more. Q wavelength of 0.03 seconds was seen in 20% of average male individuals in the posterior leads V7-V9.
Pseudo-infarct Q waves are caused by various circumstances, including physiologic or postural variations, abnormal ventricular conduction, ventricular hypertrophy, and non-coronary myocardial injury. Asymptomatic people with prominent Q waves may have had a past "silent" myocardial infarction, normal variations, or other pathologic but non-coronary etiology. Echocardiography may help in differential diagnosis (normal variants, cardiomyopathies, left or right ventricular enlargement, amyloid deposition, and so on). Failure to recognize pseudo-infarct patterns may result in "electrocardiographogenic disease" if the Q wave is a normal variant or is missing a critical clue to pathology such as hypertrophic cardiomyopathy or pulmonary embolism have very different therapeutic implications than the coronary disease.
Q Wave Diagnosis
Q wave in ECG helps in the diagnosis of the following conditions:
- Infarction of the heart
- Hypertrophic (HCM) and infiltrative myocardial disease are two types of cardiomyopathies.
- Heart rotation — Extreme clockwise or counterclockwise rotation
- Errors in lead placement, such as upper limb leads being put on lower limbs
Q Wave Symptoms
In the absence of infarction, severe myocardial ischemia may cause early QRS alterations. Atypical Q waves on the baseline ECG may not be a reliable indicator of permanently damaged myocardium.
After thrombolytic treatment, data from 695 patients with no prior historyof myocardial infarction and whose admission ECG permitted prediction of myocardial infarct size in the absence of thrombolytic therapy(Aldrich score) were seen. The presence and amount of aberrant Q waves on each patient's first ECG revealed that 53 percent of patients hospitalized within 1 hour of their symptoms had abnormal Q waves on the initial ECG. Patients with aberrant Q waves on the first ECG had greater anticipated and ultimate infarct sizes, regardless of the duration of symptoms before medication. Despite this observation, aberrant Q waves on the admission ECG did not prevent thrombolytic treatment from lowering the ultimate infarct size.
About a year after the acute cardiac attacks, leads I and III were found following anterior and posterior infarctions. In an anterior infarction, a Q wave develops at the beginning of the QRS complex in the lead I due to muscle mass loss in the anterior wall of the left ventricle; however, in a posterior infarction, a Q wave develops at the beginning of the QRS complex in the lead III due to muscle mass loss in the posterior apical part of the ventricle.
These combinations are not present in every instance of an elderly myocardial infarction. Local muscle loss and cardiac signal conduction obstruction areas might result in highly strange QRS patterns.
Q Waves No Heart Attack
Among the general population without established cardiac disease, Q-waves in the ECG is a powerful predictor of mortality or hospitalization for IHD independent of age, hypertension, diabetes, and renal function. Moreover, whilst huge Q-waves carry the worst prognosis even minor Q-waves are connected with an elevated risk. Conversely, no difference in result was detected between the anterior and posterior position of Q-waves, and both sites were linked with similarly dismal prognoses.
People Also Ask
What Happens During The Q Wave?
The Q wave shows septal depolarization. The electrical stimulus begins to depolarize the septum from left to right as it goes through the His bundle before it divides down the two branches.
What Is A Normal Q Wave?
In juvenile patients, Q waves are often detected in the inferior and left lateral precordial leads. These Q waves are usually always less than 20 ms long. In babies, the amplitude may be rather considerable (up to 14 mm).
What Does The Q Wave On An ECG Represent?
Q waves represent the early phase of ventricular depolarization. If they are extremely broad (>0.2 seconds) or abnormally deep (>5 mm), they are pathogenic. Pathologically deep but not broad Q waves are often indicative of ventricular hypertrophy.
What Causes Q Waves?
Pathologic Q waves indicate a prior myocardial infarction. A lack of electrical activity causes them. A myocardial infarction may be seen as an electrical 'hole,' since scar tissue is electrically dead, resulting in pathologic Q waves.
Conclusion
Abnormal Q waves are a typical observation in the early stages of acute myocardial infarction. There is no indication. However, aberrant Q waves are related to a worse benefit in termsof infarct size reduction following thrombolytic treatment.

Suleman Shah
Author
Suleman Shah is a researcher and freelance writer. As a researcher, he has worked with MNS University of Agriculture, Multan (Pakistan) and Texas A & M University (USA). He regularly writes science articles and blogs for science news website immersse.com and open access publishers OA Publishing London and Scientific Times. He loves to keep himself updated on scientific developments and convert these developments into everyday language to update the readers about the developments in the scientific era. His primary research focus is Plant sciences, and he contributed to this field by publishing his research in scientific journals and presenting his work at many Conferences.
Shah graduated from the University of Agriculture Faisalabad (Pakistan) and started his professional carrier with Jaffer Agro Services and later with the Agriculture Department of the Government of Pakistan. His research interest compelled and attracted him to proceed with his carrier in Plant sciences research. So, he started his Ph.D. in Soil Science at MNS University of Agriculture Multan (Pakistan). Later, he started working as a visiting scholar with Texas A&M University (USA).
Shah’s experience with big Open Excess publishers like Springers, Frontiers, MDPI, etc., testified to his belief in Open Access as a barrier-removing mechanism between researchers and the readers of their research. Shah believes that Open Access is revolutionizing the publication process and benefitting research in all fields.

Han Ju
Reviewer
Hello! I'm Han Ju, the heart behind World Wide Journals. My life is a unique tapestry woven from the threads of news, spirituality, and science, enriched by melodies from my guitar. Raised amidst tales of the ancient and the arcane, I developed a keen eye for the stories that truly matter. Through my work, I seek to bridge the seen with the unseen, marrying the rigor of science with the depth of spirituality.
Each article at World Wide Journals is a piece of this ongoing quest, blending analysis with personal reflection. Whether exploring quantum frontiers or strumming chords under the stars, my aim is to inspire and provoke thought, inviting you into a world where every discovery is a note in the grand symphony of existence.
Welcome aboard this journey of insight and exploration, where curiosity leads and music guides.
Latest Articles
Popular Articles
